Australia is advancing the future of healthcare but are we adopting it?
White paper by Neil Deacon, Managing Director of Health Advance Connect
What is the future of healthcare in Australia?
To see the future of healthcare in Australian requires that we simply look at the life sciences sector as the technologies shaping healthcare in the next 10-20 years are being developed today. Australia boasts one of the best health systems in the world (E. Schneider, 2021). Australia is also a powerhouse in life sciences and is helping to create the global future of medicine.
Key technologies transforming healthcare include:
Genomic and Precision Medicine: Advances since the Human Genome Project (2003) have made genomic testing more affordable, aiding clinical practice. Genetic insights enable precise treatments and drug companies are increasingly able to target therapies for specific genetic groups.
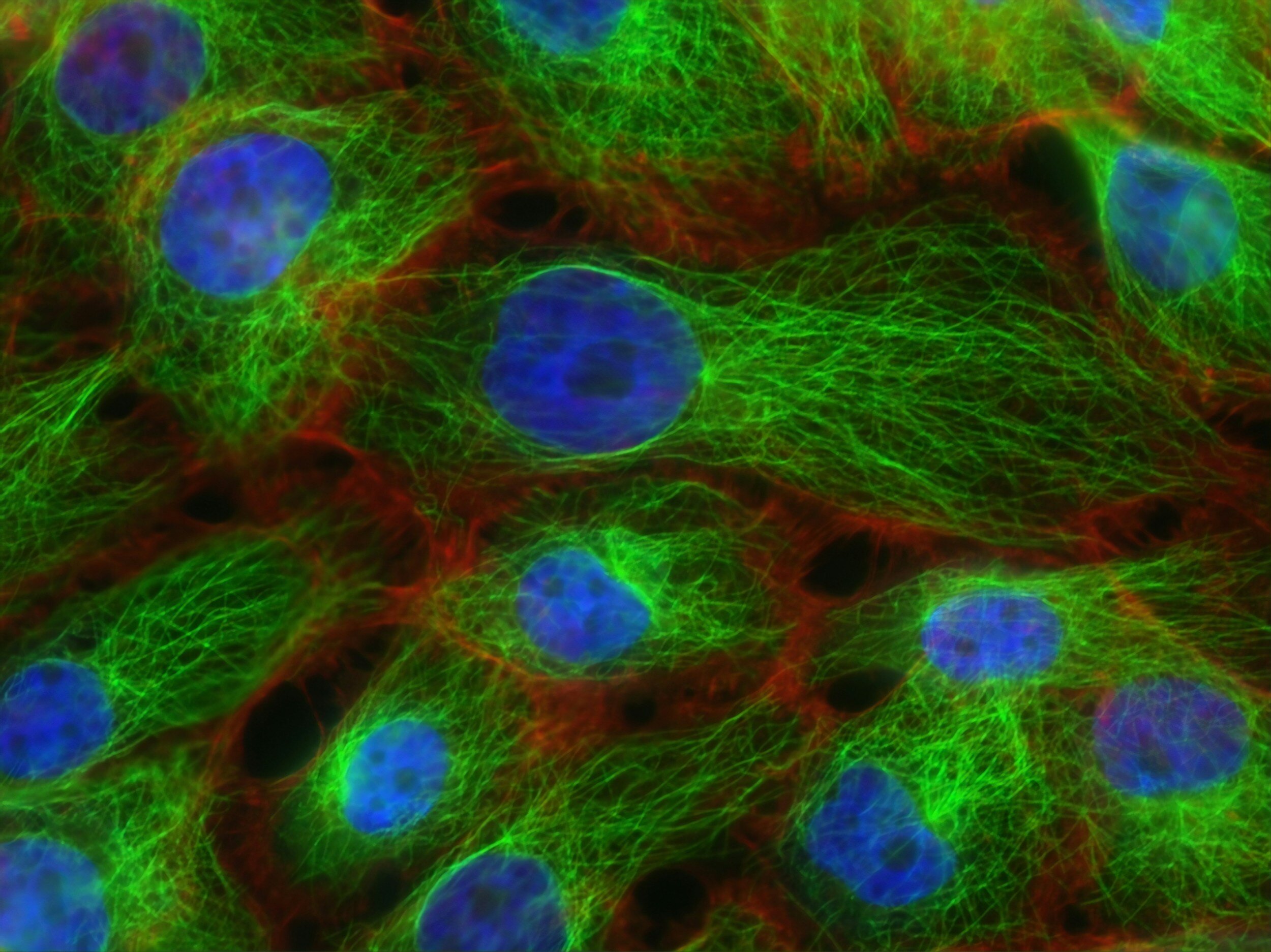
Regenerative Medicine: The focus on repairing or replacing damaged cells, tissues, or organs is increasing. Stem cell injections, gene therapies, immunomodulation, tissue engineering, and innovative treatments like platelet-rich plasma (PRP) injections and prolotherapy show significant promise in restoring function.
mRNA Vaccines: Known for countering COVID-19, mRNA vaccines deliver a small portion of genetic material to teach the body to recognise key virus protein and develop antibodies for protection. Safer and with shorter development timelines, they're poised to revolutionise disease prevention and treatment, including for influenza, HIV, and potentially cancer therapeutics (Winstead, 2022).
Digital Therapies: Digital interventions for mental health, such as internet-based cognitive behavioural therapy (CBT), smartphone apps, virtual reality, and AI-driven treatments, are proving highly effective. As the world recognizes the importance of mental health, these therapies are expected to gain prominence.
Despite these promising innovations, several roadblocks are hindering mass adoption. This paper explores these challenges, potential solutions, and the organisations leading transformative change.
How is Australia advancing the future of healthcare?
Australia's strides in Genomic Medicine
In the field of genomic medicine, Australia boasts significant achievements (Z. Stark, 2023). Australian Genomics has led a nationwide network of 100 organisations since 2016, propelling genomic testing for the diagnosis and treatment of rare diseases and cancer. They’ve showcased the efficacy of genomic testing through 19 flagship studies, collaborating with state and territory alliances.
Australian Genomics is committed to integrating genomic medicine into the nation's health systems (Australian Genomics, n.d.). This involves establishing national data resources and interoperability standards, both locally and globally. The initiative has orchestrated a cohesive strategy that has fostered a collective learning environment; enhanced workforce capabilities; updated clinical workflows; and incorporated genetic testing into established pathways. Moreover, it navigates the complex political landscape, where healthcare responsibilities are shared between federal and state/territory governments. The economic viability of genomic testing has been underlined through health economics, reinforcing the case for its broader adoption.
Australian capability in Regenerative Medicine
Australia possesses the essential elements for cultivating a thriving regenerative medicine industry, marked by cutting-edge basic and translational research and advanced manufacturing capabilities. According to AusBiotech (Biointelect, 2021), over 40 Australian companies are actively developing regenerative medicine (RM) products, complemented by more than 65 ongoing clinical trials.
At the forefront of this regenerative medicine landscape is the Australian Regenerative Medicine Institute, established in 2009 at Monash University. The institute is leading the way in unravelling the mysteries of tissue repair and replacement across five key areas: heart and muscle development and regeneration, immunity and regeneration, stem cells and regeneration, organ engineering and synthetic biology, and neural regeneration (ARMI, 2023).
Despite global challenges in regenerative medicine research and commercialisation, Australia is uniquely positioned with access to Good Manufacturing Process (GMP) certified facilities. Notably, Melbourne-based Cell Therapies, a world-leading contract development and manufacturing company, offers commercial-scale facilities capable of meeting both domestic and global demands for clinical trials and commercial production (Cell Therapies, n.d.). This strategic advantage positions Australia as a key player in the evolving landscape of regenerative medicine.
Australia’s mRNA vaccine investment
In August 2022, the Australian Government, Moderna, and the Victorian Government joined forces for a groundbreaking 10-year partnership (Prime Minister of Australia, 2022). This collaboration resulted in the establishment of an mRNA vaccine manufacturing facility at Monash University. Boasting the capability to produce up to 100 million vaccine doses annually, this facility aims to reduce Australia's reliance on imported mRNA vaccines and enhance resilience against supply disruptions.
The partnership extends beyond manufacturing, envisioning the creation of a world-class mRNA ecosystem in Melbourne. This strategic move is anticipated to attract top talent, foster collaborations with leading Australian research organisations, and expand local capabilities. Monash RNA (Monash University, n.d.), is leading research efforts on the campus and is already home to over 65 world-leading researchers, is playing a pivotal role in developing life-saving vaccines and therapeutic treatments. This collaboration signifies a significant leap forward for Australia in the realm of cutting-edge mRNA technology and healthcare innovation.
Digital therapeutics success stories
As more Australian’s are seeking help for mental health conditions (Ipsos Public Affairs, 2023), the reduction of Medicare rebate coverage from 20 to 10 sessions is intensifying challenges for Australian’s seeking help as waiting lists for psychologists and psychiatrists nationwide are getting longer and 10 sessions is often not sufficient (ABC News, 2022). However, a silver lining exists in the form of clinically validated digital tools. These innovative platforms offer effective care in a fraction of the contact time required by traditional methods, and they are backed by qualified professionals to ensure safety.
Numerous digital tools cater to various mental health conditions, including anxiety, chronic pain, and depression (Medibank, n.d.). Notably, Australian-made examples include:
My Compass: A free self-help toolkit by the Black Dog Institute, supporting mental health and wellbeing.
MindSpot: Developed by Macquarie University’s eCentreClinic, this course educates users about their symptoms and imparts proven skills to manage emotional wellbeing.
This Way Up: A collaborative effort by St Vincent’s Hospital and the University of New South Wales, offering online courses on mindfulness, chronic pain, worrying, panic attacks, and more.
What are the barriers to implementation and how do we overcome them?
There are many challenges that the health and life sciences ecosystem will collectively need to tackle over the coming years. Here are the top 8 that we’re thinking about at Health Advance Connect:
1) Growing the body of knowledge through research and development
2) Adapting regulatory capabilities and policy
3) Funding and reimbursing innovative therapies and diagnostics
4) Establishing robust and interoperable data infrastructure
5) Developing Advanced manufacturing and supply chain capabilities
6) Enabling clinical adoption
7) Securing patient acceptance
8) Addressing systematic inequities
1) Growing the body of knowledge through research and development
Significant strides have been made in advancing key technologies, yet there remains untapped knowledge crucial for enhancing precision in disease diagnosis and treatment. In Australia, from 2018 to 2021, 25,000 people underwent genomic testing, but 17,000 cases remained unsolved, indicating a 32% success rate (Biomedical Ethics Research Group, 2023). Elevating this success rate necessitates a global effort to connect genetic variations to diseases.
Australian Genomics has deployed the PanelApp platform in multiple diagnostic laboratories (Australian Genomics, n.d.), contributing to national and international initiatives like the Gene Curation Coalition. However, wider adoption, possibly in collaboration with global entities like Genomics England and US NIH initiatives ClinVar and ClinGen, is essential for efficient gene-disease relationship establishment.
Beyond leveraging research knowledge, Australia should actively partake in global research endeavours. Being a leader in innovative research not only creates high-skilled jobs but also provides early access to experimental therapies for Australian patients through clinical trials. This positions Australia to be at the forefront of adopting and deploying novel technologies globally.
While Australia possesses strong research capabilities, increased investment is imperative to secure a prominent global position. AusBiotech's vision for expanding regenerative medicine (Research Strategies Australia, 2021), coupled with similar initiatives in mRNA technologies and digital therapeutics, can solidify Australia as a world leader. It can also enable Australia to harness its robust research credentials for the benefit of its citizens.
25,000
genetic tests completed from 2018 to 2021
9,000
resulting in diagnosis (32%)
17,000
tests unsolved (68%)
Figure 1: Unsolved rate demonstrates a significant gaps in our understanding that will be addressed by domestic and global research
2) Adapting regulatory capabilities and policy
The shift from blockbuster pharmaceuticals to precise treatments - encompassing small molecules, biologics, regenerative medicine, and digital therapies - heralds a new era of safer and more effective patient care. However, this evolution poses challenges for companies seeking marketing authorisations and the regulatory bodies responsible for approval (A. Breckenridge, 2016).
As precision medicines replace broad-spectrum therapies, the landscape demands more treatment options targeting smaller patient cohorts. Originators face the task of submitting a higher volume of applications for expansive product portfolios, necessitating faster processes than the prolonged timelines seen with blockbuster drugs. While the previous norm involved substantial investments over years, the upcoming generation of products, with individually lower sales projections, requires a scaled-back, justifiable approach to regulatory submissions. This calls for the adoption of faster filing methods, incorporating technologies like AI, and regulators to accelerate review and approval processes without compromising their integrity.
Regulators, such as the TGA, grapple with evaluating applications involving novel technologies like cell therapies using patients' stem cells, diverging from the familiar terrain of small molecules and biologics. To prevent unacceptable backlogs that impede the approval of life-saving therapies, regulators must prioritize applications effectively, collaborate with originators to streamline processes, and align with global regulatory agencies to standardize submission requirements and expedite decision-making processes. This harmonization effort is crucial to ensure timely access to innovative treatments without compromising safety and efficacy.
Figure 2: FDA drug regulation activity has been steadily rising over the last decade (Source: FDA, HAC analysis) - we expect it’s a similar trend for the TGA!
3) Funding and reimbursement of diagnosis and innovative treatment
To ensure a health system that can consistently deliver cutting-edge treatments, attention must be directed toward securing funding for both establishing capabilities and reimbursing the appropriate clinical use of emerging technologies. While continued investment in research is crucial, it is equally essential to channel resources into building robust data infrastructure, optimising supply chains, and enhancing analytic capabilities.
Reanalysis of genetic tests is a pivotal aspect of leveraging new knowledge to diagnose previously unsolved cases. However, the current human capacity falls short, with only 5% of the 17,000 unsolved cases reanalysed between 2018-2021 (Biomedical Ethics Research Group, 2023). Additional investment is imperative to expand genetic analysis capacity nationwide and to automate analysis and reanalysis processes, alleviating the strain on limited human resources.
Moreover, the cost of innovative technologies, aside from mRNA vaccines and scalable digital therapies, is expected to be higher than existing medications. While the efficacy of these treatments and their positive impact on patients' lives in many cases form a favourable health economic case (A Nagpal, 2019), a short-term affordability challenge exists. Health systems must navigate how to finance these novel treatments without exacerbating existing inequalities of access. In the Australian context, achieving new funding models necessitates collaborative efforts across federal and state governments to ensure equitable access and sustainability.
4) Establishing robust and interoperable data infrastructure
Navigating the delicate balance between data security and efficient data sharing in healthcare has been a challenge. Seamless sharing of health data between patients and providers can enhance patient experiences, reduce redundant investigations, and minimize medical errors. With the increasing prominence of genomic medicine, this challenge becomes more pronounced due to the vast size of genomic data and the need for secure storage and transfer to approved recipients.
Australia faces hurdles in genomic data management due to siloed data practices and a lack of interoperability standards. However, promising solutions are emerging. Genomical, supported by the Melbourne Genomics Health Alliance, is making significant strides in the secure storage, authorised access, and meaningful use of genomic data (Genomical, n.d.). The platform also establishes data standards for Australian medical laboratories, expediting genomic testing and enabling efficient analysis and reanalysis. While currently adopted by six Victorian healthcare providers, nationwide implementation of such a standard platform would greatly enhance Australia's capacity for collecting, analysing, and managing genomic data.
Additionally, the federal government's plan to legislate digital health standards signals a significant step forward (Knibbs, 2023). Drawing inspiration from the US 21st Century Cures Act, this legislation aims to compel Australian healthcare vendors to adhere to common data standards within a defined timeframe. If the federal government follows through assertively, Australia could witness widespread compliance with a single set of data standards among vendors by the end of the decade. This legislative push has the potential to revolutionize the landscape of healthcare data management in the country.
5) Developing advanced manufacturing and supply chain capabilities
Ensuring advanced manufacturing capabilities with GMP certification is crucial for meeting the growing demand for cell and gene therapies as well as mRNA technologies. Melbourne, with establishments like Cell Therapies (Cell Therapies, n.d.) and Moderna's investment in the Monash precinct (Prime Minister of Australia, 2022), is currently at the forefront of developing such capabilities.
However, the imminent surge in demand could quickly surpass the existing supply capacity. To address this, substantial investment is necessary to scale up advanced manufacturing in Australia. Moreover, considering that many therapeutic interventions require proximity to the manufacturing site for patient administration, relying too heavily on Melbourne would create accessibility challenges and strain on local hospitals. Therefore, it becomes imperative to establish GMP-certified advanced manufacturing facilities across the country, initially in other state and territory capitals, and potentially extending to regional deployment.
For mRNA technologies, the unique challenge lies in the inevitable fluctuations in demand. Facilities, like the Moderna site, need to effectively manage the scaling up and down of production, driven by seasonal variations in flu vaccinations, potential pandemic waves, and expanding clinical applications such as therapeutic vaccines for cancer treatment.
Additionally, the cold-chain distribution requirements for certain mRNA technologies, especially in a vast and hot country like Australia, present logistical challenges. Addressing these challenges will be vital to ensuring the effective and equitable distribution of these advanced therapies across the country.
Figure 3: Advanced Manufacturing site locations (Source AusBiotech, adapted by HAC)
6) Enabling clinical adoption
Precision medicine, a concept deeply rooted in the quest for a deeper understanding of disease and more effective treatments, has evolved rapidly over the past decade. This has been particularly so with the increased availability of genomic information. The acceleration of new diagnostics and treatments introduces a richness of options and unprecedented complexity to the healthcare landscape.
This complexity poses significant challenges for clinicians and necessitates a re-evaluation of how our health system is structured. Adapting to these challenges requires providing the necessary support and implementing systemic changes to empower clinicians and patients in the dynamic environment of healthcare and health technology.
Examining diabetes management as an illustration, the shift from one insulin product in 1982 to 18 different insulin products and a myriad of other therapeutic options by 2020 exemplifies the increasing choices clinicians face (see Figure 4).
This clinical complexity is magnified when incorporating genomic data, with its growing library of linkages between genetic variants, diseases, and therapies. Furthermore, clinicians need to consider non-chemical interventions like digital therapeutics, shown to be effective and safer in areas such as chronic pain management.
To address this complexity, tools supporting clinicians in managing precision medicine and the diverse array of available treatments are crucial. Integration models that bridge the expertise of general practitioners with the specialised knowledge in tertiary centres are essential for effectively navigating the complexities of precision medicine. This collaborative approach will ensure that clinicians can leverage the full range of available therapies and provide optimal care to patients.
Figure 4: Increase in treatment options for Diabetes since 1982 (Source: FDA, HAC analysis)
7) Securing patient acceptance
Addressing patient acceptance is crucial for the success of advanced medical treatments and technologies. The challenges of hesitancy and vociferous opposition, highlighted during the COVID-19 vaccination rollout, underscore the importance of overcoming misinformation and building trust.
While the COVID-19 vaccination effort in Australia achieved an impressive 82.7% completion rate (Centers for Disease Control and Prevention, 2024), anti-vaxx messaging and vaccine hesitancy remain a growing concern (Tsirtsakis, 2021). Misinformation, particularly surrounding the rapid development of mRNA vaccines, poses a significant threat to public health. To counter this, it is essential to provide accurate scientific information and address concerns, emphasising the positive differentiators of advanced medical technologies.
Similar challenges have been witnessed in the adoption of regenerative medicine and digital therapeutics. Ethical concerns and media attention contribute to hesitancy in regenerative medicine (N. King, 2014), while low acceptance of digital therapeutics is mostly linked to low performance expectations among both patients and healthcare professionals (P. Philippi, 2021) – See Figure 5.
To enhance patient acceptance, there is a need for widespread dissemination of accurate information directly to consumers and through healthcare professionals. However, there are no easy answers for tackling misinformation and it is likely that whole-of-government approaches are needed to build the health and media literacy required. We can take inspiration from countries like Finland that prioritises media literacy in its education system (Patil, 2021). Empathy towards hesitant individuals, coupled with education from an early age, can empower individuals to distinguish between reliable health information and misinformation.
Building trust in governments and institutions is fundamental. Transparent communication and evidence-based advice contribute to fostering confidence in advanced treatments and technologies. By addressing these aspects collaboratively, we can pave the way for widespread acceptance and successful implementation of innovative medical approaches.
Figure 5: Unified Theory of Acceptance and Use of Technology –UTAUT (Source: Venkatesh et. al, 2003, adapted by HAC)
8) Addressing systemic inequities
Addressing systemic inequities is a critical challenge facing Australia, with disparities in access and outcomes evident across various demographic groups. These disparities negatively impact those in lower socio-economic groups, women, people from CALD backgrounds, people with disability, and people living in rural and remote areas, but the most pronounced difference is between non-Indigenous and Indigenous communities.
Historical legacies of colonialisation and policies implemented over the past two centuries have limited opportunities for education, employment, social participation, housing, and healthcare access for Indigenous populations. Overrepresentation in the criminal justice system compounds these challenges, resulting in poorer health outcomes. The most glaring discrepancy is seen in life expectancy, where Indigenous Australians live 7.8-8.6 years less than their non-Indigenous counterparts (Australian Government, 2020). We also see that more Indigenous people are living with disability, the Royal Commission in Violence, Abuse, Neglect and Exploitation of People with Disability noted that 35% of Indigenous people under the age of 65 had disability, which is 3 times higher than the non-Indigenous population (Disability Royal Commission, 2023).
While advances in medicine hold the promise of improving life expectancy and quality, ensuring equitable access to these benefits is a pressing concern. Affordability and supply issues may exacerbate existing disparities. Although advanced medical centres are typically located in metropolitan areas, the responsibility falls on governments and health departments to ensure that these benefits are accessible to all Australians, regardless of their geographical location or financial means.
Addressing this complex issue requires collaborative efforts between governments, national bodies such as NACCHO (National Aboriginal Community Controlled Health Organisation), and local Aboriginal and Torres Strait Islander leaders across the country. Comprehensive understanding of national and local barriers to access and acceptance of treatments is essential to create effective, culturally sensitive solutions that promote health equity for all Indigenous peoples in Australia.
Figure 6: Key statistics in Indigenous vs Non-Indigenous inequity (Sources: Closing the Gap report, Australian Institute of Health and Wellbeing, Australian Bureau of Statistics, and the Disability Royal Commission)
Where to from here?
The future of life sciences and healthcare in Australia is promising, with exciting advancements on the horizon. However, there are considerable challenges which need to be addressed via focused and strategic approaches.
Health Advance Connect has been established to collaborate with health and life sciences leaders and offer support to craft and implement effective strategies to navigate these challenges.
We recognise four crucial types of strategies for success:
Investment Strategies: Federal and state governments play a pivotal role in making coherent funding choices. Investing in capabilities and infrastructure across the country and throughout the value chain is essential to produce and deliver cutting-edge therapies for all Australians.
Collaboration Strategies: Many challenges in the healthcare landscape cannot be tackled by individual organisations alone. Forming alliances and consortia is necessary to pool expertise and resources, fostering collaboration to achieve common goals.
Growth Strategies: While some challenges are already being addressed, there is a need for strategies to scale these efforts to meet the broader demand. Successful enterprises must navigate growth journeys to expand their impact.
Organisational Change: The operational landscape of the next generation of medicine requires organisational changes across the ecosystem. Effective change management starts with the right strategic direction.
At Health Advance Connect, we bring experience in all these strategy types and more. Together, we can navigate the exciting future of healthcare and life sciences in Australia.
Final comment
At Health Advance Connect we value humility; we are deeply interested in the Australian Health and Life Sciences ecosystem, and we know there is always more to learn. We are eager to hear other perspectives about the successes, challenges and solutions for our Australian healthcare system and life sciences industry. If you would like to share yours, please reach out.
References
A Nagpal, R. M.-B. (2019). Economic Evaluation of Stem Cell Therapies in Neurological Diseases: A Systematic Review. Value in Health, 254-262.
A. Breckenridge, H.-G. E. (2016). Precision medicine and the changing role of regulatory agencies. Nature Reviews Drug Discovery, 805-806.
ABC News. (2022, December 13). Seeing a psychologist on Medicare? Soon you'll be back to 10 sessions. But we know that's not enough. ABC News.
ARMI. (2023). our groups. Retrieved from ARMI: www.armi.org.au/our-groups
Australian Genomics. (n.d.). panelapp-australia. Retrieved from australian genomics: https://www.australiangenomics.org.au/tools-and-resources/panelapp-australia/
Australian Genomics. (n.d.). What we do. Retrieved from https://www.australiangenomics.org.au/
Australian Government. (2020). Closing The Gap Report 2020. Canberra: Australian Government.
Biointelect. (2021). The Regenerative Medicine Value Chain. Melbourne: AusBiotech.
Biomedical Ethics Research Group. (2023, July 31). Automation of reanalysis of genomic sequencing data. Retrieved from YouTube: https://www.youtube.com/watch?v=Bsl0O4hjcNc
Cell Therapies. (n.d.). About Cell Therapies. Retrieved from https://celltherapies.com/about/
Cell Therapies Pty Ltd. (2021). Australia’s Regenerative Medicine Manufacturing Capacity and Capability. Melbourne: AusBiotech.
Centers for Disease Control and Prevention. (2024, January 24). Global-vaccinations. Retrieved from COVID data tracker: https://covid.cdc.gov/covid-data-tracker/#global-vaccinations
Disability Royal Commission. (2023). Final report Vol 3: Nature and extent of violence, abuse, neglect and exploitation. Canberra: Royal Commission into Violence, Abuse, Neglect and Exploitation of People with Disability.
E. Schneider, A. S. (2021). Mirror, Mirror 2021: Reflecting poorly, healthcare in the US compared to other high-income countries. The Commonwealth Fund.
Genomical. (n.d.). What is Genomical? Retrieved from Genomical: https://genomical.com.au/about-genomical/what-is-genomical/
Ipsos Public Affairs. (2023). Report to the Nation 2023. Mental Health Australia.
Knibbs, J. (2023, March 16). Govt will legislate to drive digital health changes. Wild Health.
Medibank. (n.d.). digital tools for mental health. Retrieved from medibank: https://www.medibank.com.au/health-support/mental-health/articles/digital-tools-for-mental-health/
Monash University. (n.d.). mrna. Retrieved from Monash Australia: https://www.monash.edu/mrna
N. King, J. P. (2014). Ethical issues in stem cell research and therapy. Stem Cell Research & Therapy.
P. Philippi, H. B.-H.-M. (2021). Acceptance towards digital health interventions - Model validation and futher development of the Unified Theory of Acceptance and Use of Technology. Internet Interventions.
Patil, R. (2021, September 24). An Evolving Fight: Finland's Success in Tackling Misinformation and what the World can Learn. Retrieved from Europe Monitor: https://www.theeuromonitor.com/an-evolving-fight-finlands-success-in-tackling-misinformation-and-what-the-world-can-learn/
Prime Minister of Australia. (2022, August 15). Media. Retrieved from Prime Minister of Australia: https://www.pm.gov.au/media/homegrown-vaccines-way-australia
Research Strategies Australia. (2021). Regenerative Medicine in Australia. Melbourne: AusBiotech.
Tsirtsakis, A. (2021, May 18). Online Australian anti-vaxx groups grow by nearly 300%: Report. newsGP (RACGP).
Venkatesh, V. (2003, September). User Acceptance of Information Technology: Toward a Unified View. MIS Quarterly, 425-478
Winstead, E. (2022, January 20). mrna-vaccines-to-treat-cancer. Retrieved from NIH: National Cancer Institute: https://www.cancer.gov/news-events/cancer-currents-blog/2022/mrna-vaccines-to-treat-cancer
Z. Stark, T. B. (2023). Australian Genomics: Outcomes of a 5-year national program to accelerate the integration of genomics in healthcare. American Journal of Human Genomics, 419-426.